Data-driven maternal health literacy promotion and a postscript on its implications
Abstract
Scientific discovery and global health policy are moving health literacy promotion and maternal-child health from the fringes of research and public health to the forefront of healthcare reform [Matern Child Health J. 18 (2014), 344–365]. In 2011 the United Nations General Assembly adopted the Shanghai Declaration [Lancet 378 (2011), 566–567]. The Declaration highlights new understanding of the origins of health and disease in early development. It calls on all nations to apply this knowledge to reduce the burdens of chronic disease and related disparities worldwide. The Declaration recommends a specific intervention strategy: promote health literacy across the life course, particularly in parents and children, and empower women.
This article explores findings and implications of the Life Skills Progression Maternal Health Literacy studies. These LSP-MHL studies evaluated implementations of an intervention designed to promote health literacy in parents and empower women in the U.S. First, the article reports findings of the most recent of five published LSP-MHL studies with discussion of its implications for future work in this line of inquiry. A postscript highlights two of many implications of the LSP-MHL intervention studies for health literacy research in the third era of modern healthcare.
1.Introduction
Two research goals guided the present study. First, the authors aimed to assess progress toward maternal health literacy (MHL) in the context of everyday life among disadvantaged mothers of children aged 0 (pregnancy) to 3 years in the U.S. The authors hypothesized that MHL scores would show improvement and that the social determinants of health would influence progress. The second aim was to explore how data visualization methods might increase understanding of how MHL develops and what supports or impedes improvement. Of particular interest are visualizations that could facilitate routine use of data by community-based, non-scientist health and social services providers as a guide to tailoring intervention for particular families and circumstances.
1.1.Overview of the article
Section 2 of this article describes a sociocultural model of maternal health literacy (MHL) in contrast to the dominant clinical model and identifies gaps in the literature. Section 3 Methods details the research design, sample, intervention, measurement, and analytical methods of the present study. Section 4 Results presents findings along with data visualizations and notes on how to interpret them.
Section 5 Discussion considers results of this study confirming and challenging previous findings. New findings and data visualizations confirm that MHL improvement can be maintained and evolve over extended periods of changing HL needs and demands. Section 5.2 describes the utility of combined contextual and intermediate outcomes data to reveal pathways to progress and guide intervention tailoring. The negligible influence of reading skill in MHL improvement is discussed in Section 5.3. Section 5.4 outlines evidence that promoting MHL can reduce disparities due to literacy, young age and mental health. Discussion of MHL as an empowerment strategy, and an illustration of how data visualization documented health empowerment in the study population follow in Section 5.5. Section 5.6 examines the feasibility of data-driven practice in which practitioners routinely use data to personalize intervention. Next, in Section 5.7 an important new finding is discussed: the powerful influence of the social determinants of health on MHL as illustrated by the “Web of Interaction”. Section 5.8 suggests MHL promotion can be scaled up through existing home-based interventions. Section 5.9 notes that new findings challenge earlier research which avoided the complexity of home contexts in favor of precision and parsimony. Embracing the complexity revealed pathways to progress and increased understanding of MHL improvement and empowerment. Section 6 suggests future directions for LSP-MHL research and practice.
The Postscript, presents a review of five published LSP-MHL studies and discusses two of their many implications. Section 7 outlines a brief history of the evolution of modern healthcare and describes the Developmental Origins of Health and Disease (DOHaD) and related theories that underpin the MHL concept, the LSP, and calls to promote health literacy as a pragmatic intervention to reduce disease and disparities. These theories have ushered in the third era modern healthcare and positioned maternal-child health and MHL at the very foundations of personal and public health worldwide. Section 8 outlines specific health promotion strategies shown to promote MHL and empowerment. Section 9 describes a comprehensive evaluation framework for health literacy interventions in child health. Section 10 closes the postscript with suggested topics for multidisciplinary dialogue on the challenges and promises of data-drive practice, evidence-based evaluation, and theory-based research in health literacy promotion, particularly in maternal and child health.
2.Maternal health literacy: Personal asset, life skills, empowerment strategy
Maternal health literacy is a determinant of child [1] and adult health [9] and a source of health disparities [14] worldwide. In accordance with earlier research, the authors operationalized MHL using the World Health Organization definition [19] made specific to mothers [26]:
the cognitive and social skills which determine the motivation and ability of mothers to gain access to, understand, and use information in ways that promote and maintain their health and that of their children.
In this sociocultural model, MHL is understood as a personal and community asset [20], a life skill required to navigate health systems and everyday choices that influence health [19]. Promoting MHL is an empowerment strategy to increase mothers’ control over personal and child health [13] by increasing their capacity to function in three domains: 1) disease treatment and healthcare, 2) disease prevention and health protection, and 3) health promotion [34]. Each of these domains presents a different set of health literacy tasks in different contexts requiring different combinations of skills.
Most health literacy research, especially in the United States, has addressed the disease treatment and healthcare domain exclusively. Studies have taken a clinical approach focused on patients’ lack of reading and numeracy skills needed to understand information related to clinical encounters. Scholars have described this construct as health-related literacy [4,21]. Associations are established between low health-related literacy and adverse clinical outcomes. However, results are mixed and the pathway linking reading skills to outcomes is unclear, especially the link between mothers’ reading ability and child health outcomes [8]. Largely due to inadequate measures, intervention studies remain rare [1], especially community-based interventions customized to diverse low-literacy populations [28], interventions focused on improving skills [6], and interventions in child health [8]. Health literacy and empowerment rarely have been investigated together; and scant attention has been paid to the role of the social determinants of health in heath literacy. The present study addresses these gaps in the evidence base.
3.Methods
3.1.Design
This study is a secondary analysis of a U.S. Agency for Healthcare Research and Quality/National Institutes for Health database combined for AHRQ/NICHD grant #R03HD055618-02.
3.2.Sample
Participating programs, parents and the intervention are described in detail elsewhere [32]. Briefly, of 2395 socio-economically disadvantaged primary caregivers in our database, 98.5% are mothers. Their average age is 24.2 years (sd 0.16); 37% are African American, 32% Caucasian, 18% Hispanic/Latino, and 13% other or unknown. A literacy screen validated with parents of children < age 6 in primary care [5] indicated 27% of the mothers are below-average readers (⩽6th grade level) who would benefit from adult education. Children (
3.3.Intervention
The intervention was implemented by 69 home visitors in six programs representing five U.S. national models of home visitation. Home visiting is a preventive intervention to promote maternal-child health and support healthy child development and school readiness. The participating sites are located in California, Montana, Indiana, Georgia, and Virginia. The home visitors were paraprofessionals, public health nurses, nurse case managers, and social workers. These service providers addressed health and social issues together during visits to families in their homes for one to two hours weekly or monthly, for six to 36 months. The service providers were trained in health literacy and empowerment concepts. They integrated into their usual health education and skills development activities an empowerment approach to developing interactive and critical skills.
3.4.Measures – Life Skills Progression instrument: LSP data guides practice
As part of their usual activities, the participating service providers collected data on mothers’ preventive and healthcare-related practices and surrounding family conditions at baseline and six-month intervals for up to 36 months using the LSP [39]. To evaluate MHL and monitor improvement, the authors used the LSP measures of information seeking, use of health services and community resources, health behaviors, preventive practices, and maintenance of safe environments. In other words, they monitored changes in the degree to which mothers produced the theoretically identified consequences of increased health literacy: improvement in health services utilization, risk behaviors, and selfcare [36]. Two previously validated scales derived from the LSP assess different aspects of maternal health literacy [30,32].
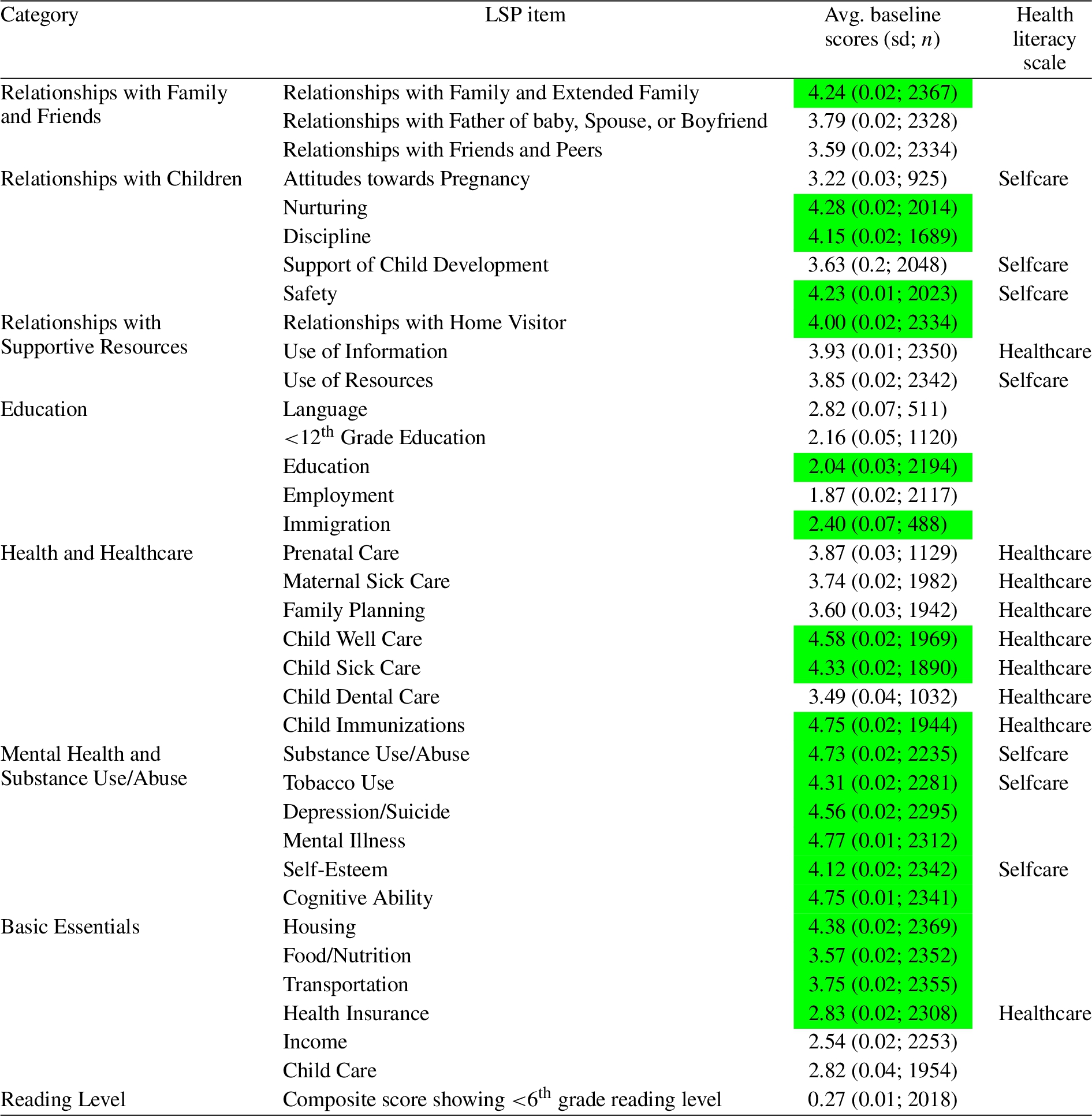
The Healthcare Literacy scale (HcL) combines nine LSP item scores to evaluate mothers’ use of information and healthcare for the dyad in the previous 6-month period. Sequential changes in the scale score indicate changes in skills that pertain to participation in healthcare. The Selfcare Literacy scale (ScL) combines seven LSP item scores to evaluate mothers’ management of personal and child health at home. The ScL scale score indicates skills that pertain to everyday choices, preventive practices and health promoting behaviors that influence family health. See Table 1. In addition, to tie this study to research on health-related literacy, the authors used the LSP’s optional health-related literacy screen [5].
Table 1
Summary of LSP items, categories, and MHL scales. This table provides a listing of the items in the Life Skills Progression (LSP) instrument and their organization by categories and inclusion in Healthcare Literacy or Selfcare Literacy scale scores. Baseline scores for each item are listed, and the green box indicates that the average score at baseline was in the target range for a given LSP item
3.5.Analysis
Analysis and visualizations were completed with STATA [35] and RStudio [27]. In addition to descriptive statistics exploring changes in LSP item scores, paired t-tests were conducted to assess changes in MHL scores from baseline to 6 months of service, 6 to 12 months, 12 to 18 months, and from 18 to 24 months. Among mothers with three or more assessments, repeated-measures ANOVA was conducted to evaluate changes in LSP scores. Average MHL scale score, and LSP item score differences for each time period were calculated among mothers with scores for both time points, and are visualized as a heatmap. Hierarchical cluster analysis shows LSP item scores that display the same pattern of change over time. Bonferroni-adjusted pairwise correlations at baseline illustrate relationships between LSP items as a chord diagram.
4.Results
4.1.MHL scores improved continuously
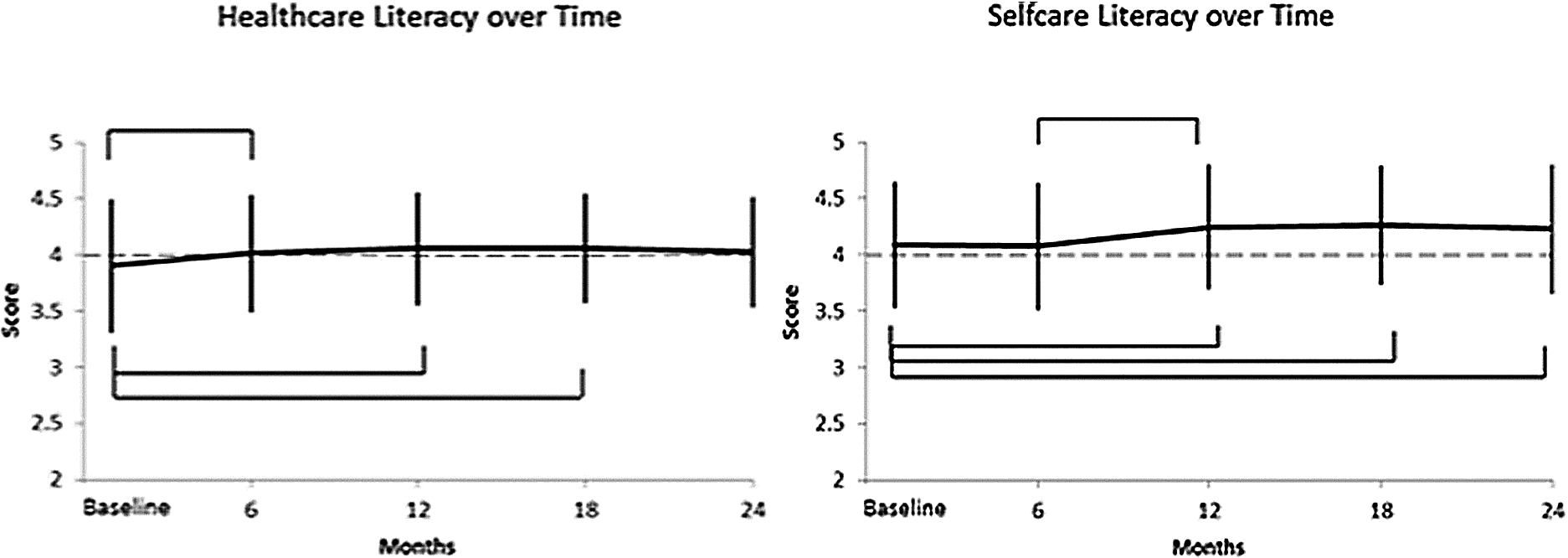
From initiation of service to 24 months, overall, Healthcare Literacy scores improved from below target into target range (mean score 3.9 to 4.03;
Fig. 1.
Average maternal Healthcare literacy and Selfcare Literacy scores over time. The bars indicate that the change in score is statistically significant (
4.2.Heatmap shows what changed when
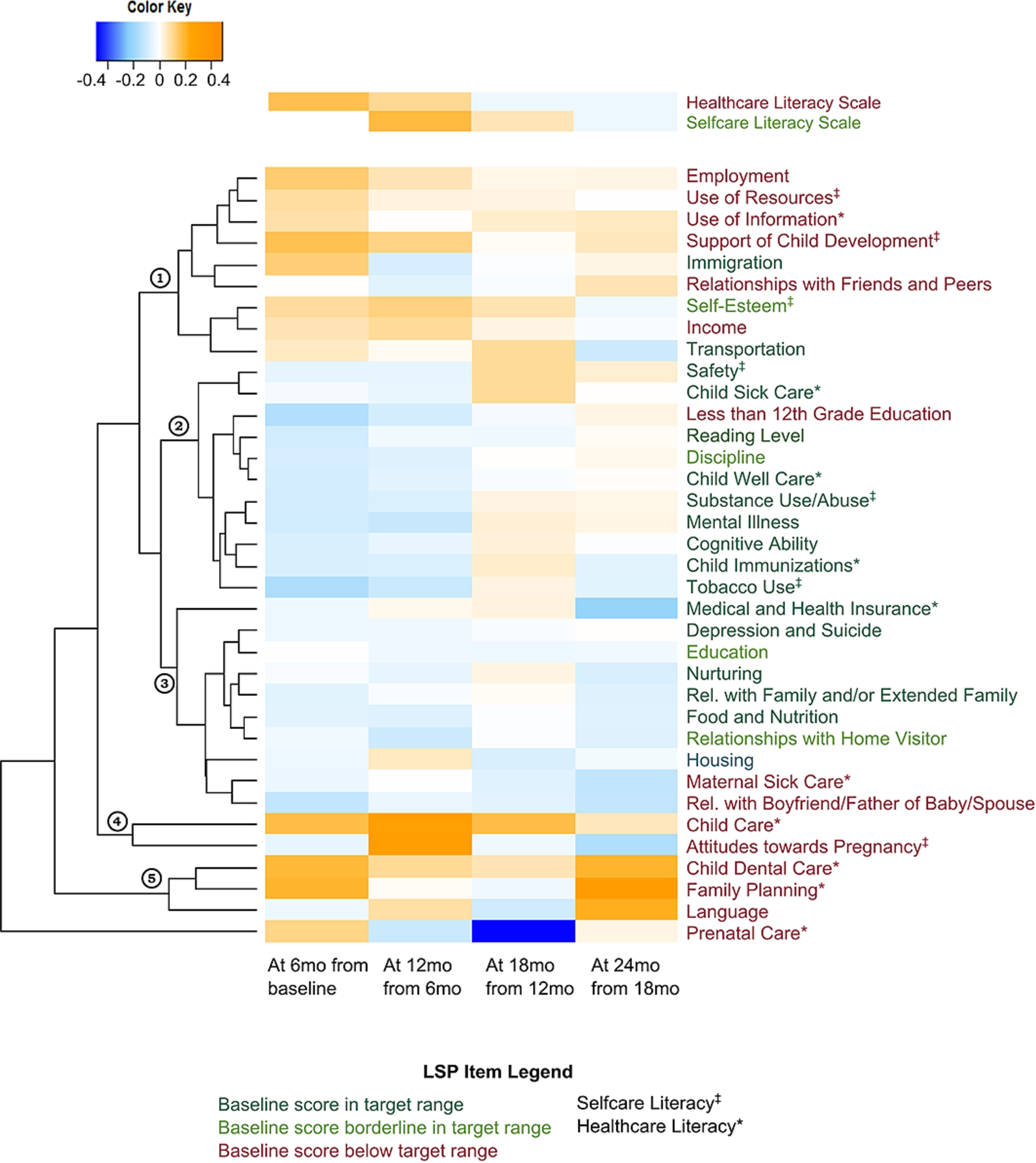
Figure 2 illustrates the rate of average score change for each LSP item. The heatmap converts data to color to visualize patterns of change. Variations in color and intensity highlight the average differences in item scores from one observation to the next among mothers with both observations (e.g. “At 6 mo. from baseline” shows the average score change among mothers with both a baseline and 6-mo observation). Observation points should not be confused with child age. Service typically began late in pregnancy or shortly after birth, so that at the end of 12 months of service the child may be aged 6 to 15 months. Orange indicates an increase in the overall average score from the previous observation; blue indicates a decrease. More intense color indicates greater score change since the previous observation. White indicates score maintenance; that is, no change between observations.
The upper heatmap showcases the two MHL scales, Healthcare Literacy and Selfcare Literacy. Healthcare Literacy shows early and steady improvement followed by maintenance. For Selfcare Literacy, the heatmap shows delayed improvement followed by maintenance. The lower heatmap shows patterns of change for each LSP item. For example, in Prenatal Care (PNC), the last item listed, light orange in the leftmost column shows that in the first 6 months, prenatal care participation increased moderately from baseline as pregnant mothers enrolled in PNC. In the 6–12-months period, light blue indicates a moderate decline in PNC participation as some mothers gave birth and ended PNC. By 12–18 months of service, dark blue indicates a strong decline as the last of those who were pregnant at baseline delivered and obtained (or missed) a postpartum check-up. In the 18–24 month period, white indicates the near zero level of the previous observation was maintained, suggesting that mothers practiced birth spacing, an important intermediate outcome on the path to ultimate clinical outcomes.
Fig. 2.
Differences in average scores over time. This heatmap highlights changes in average LSP scores at each 6 month interval, calculated among mothers with both observations (e.g. 6 mo to Baseline is based on mothers with both baseline and 6-mo observation scores). The Healthcare Literacy score shows early ample progress, followed by modest progress and near-maintenance. The Selfcare Literacy score shows delayed ample progress, followed by modest progress and near-maintenance. The dendrogram clusters the LSP items by pattern, providing insight into items that “behave” similarly over time. 1 ◯ bracket shows LSP items that improved early and slowly continued to improve; 2 ◯ bracket shows LSP items that demonstrated early slight decreases followed by modest improvements; 3 ◯ bracket shows LSP items with predominantly score maintenance or minor changes; 4 ◯ bracket shows LSP items with substantial and intermittent improvements; 5 ◯ bracket shows LSP items with substantial and ongoing improvements; last line shows an LSP item with a fluctuating progress.
4.3.Mothers overcame multiple challenges
The heatmap also offers insight into challenges disadvantaged U.S. mothers faced to maintain health, and the timing and degree of improvements they achieved. Table 1 shows that overall 16 life skill indicators were rated below target range at baseline, and another four were borderline in target range (within 0.15 of target cut-off). Items rated below target range (challenges) include MHL indicators: Support of Child Development, Use of Information, Use of Resources, Prenatal Care, Maternal Sick Care, and Child Dental Care; along with contextual factors: Relationships with Father of Baby, Spouse, or Boyfriend; Relationships with Friends and Peers; Attitudes towards Pregnancy; Language; <12th Grade Education; Employment; Income; Child Care; and Reading Level. Of these 16 items, 12 demonstrated substantial improvement in the first year of service. Four remained below target: <12th Grade Education (rated for school-age mothers only), Maternal Sick Care (closely related to insurance status), Relationships with Father of Baby, Spouse, or Boyfriend; and Reading Level. Of the four borderline items (Self-Esteem; Discipline; Education; and Relationships with Home Visitor), average Self-Esteem scores showed continuous improvement throughout service.
4.4.Dendrogram shows factors that changed together
The dendrogram (numbered brackets on the left of Fig. 2) clusters together items that display a similar pattern of change. Each of the numbered large brackets has sub-brackets that refine the groupings to smaller and more similar patterns. Here the authors discuss the major themes from the dendrogram, acknowledging nuanced differences within each bracket.
The top bracket 1 ◯ shows LSP items that improved early and continued to improve at a slower rate. This bracket includes MHL indicators: Use of Information, Use of Resources, Self-esteem, and Support of Child Development; along with contextual factors that influence or are influenced by them: Immigration, Relationship with Friends and Peers, Employment, Income, and Transportation.
The next bracket 2 ◯ shows items that demonstrated early slight decline in scores followed by modest score improvements including MHL indicators: Safety, Child Sick Care, Tobacco Use, Substance Use/Abuse, and Child Well Care; along with Discipline and contextual factors: Mental Illness, Cognitive Ability, Less than 12th Grade Education.
The third bracket 3 ◯ highlights items that showed predominantly score maintenance or minor shifts in average scores for each period, including MHL indicators: Child Immunizations, Parent Sick Care, and Medical/Health Insurance; along with contextual factors: Housing, Depression/Suicide, Education, Nurturing, Relationships with Family and/or Extended Family, Food/Nutrition, Relationships with Home Visitor, and Relationships with Boyfriend/Father of the Baby/Spouse.
The last brackets 4 ◯ and 5 ◯ show items that improved strongly early and sporadically, with slight decreases or score maintenance including MHL indicators: Child Dental Care, Prenatal Care, Child Care, Attitudes towards Pregnancy, and Family Planning; along with Language.
4.5.Correlations weave a web of interaction
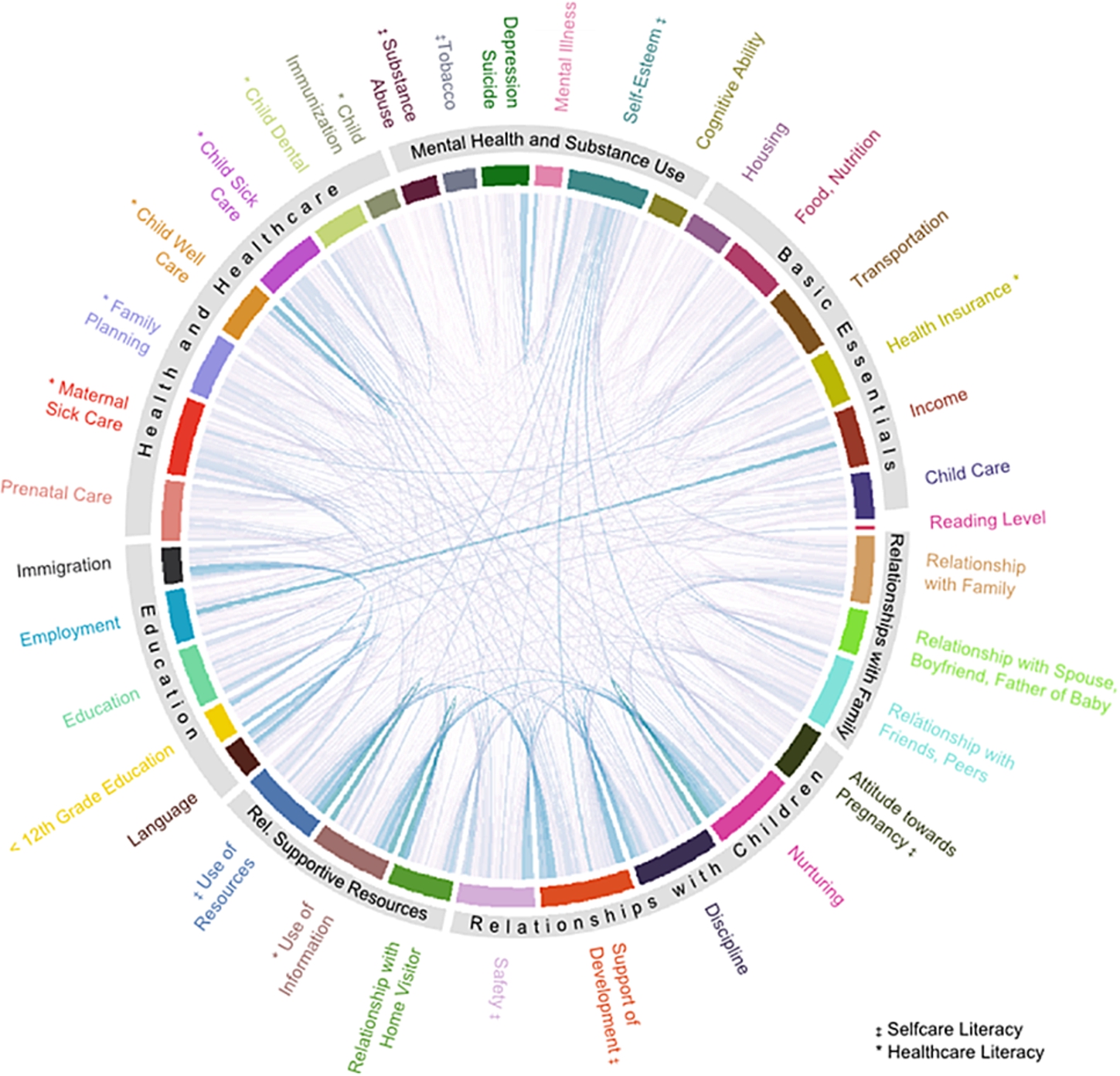
Figure 3 highlights the relationships among LSP items mapped in a chord diagram. The items with the most and strongest correlations include MHL indicators: Self-esteem, Use of Resources, Use of Information, Maternal Sick Care, and Child Sick Care; along with contextual items in Basic Essentials; Relationships with Family, Friends and Peers; and Relationships with Supportive Resources. The factors with the fewest and smallest correlations are Language, Immigration, Less than 12th Grade Education, and reading level.
Fig. 3.
Web of interaction. The Bonferroni-pairwise correlations mapped in a chord diagram highlight the complexity of health literacy concepts through their relationships with each other. The chord diagram draws a link for each significant pairwise correlation. The relative width of the colored bar representing each LSP item is proportional to the number of correlations with that item; a wider bar indicates the item has more correlations and/or stronger correlations than an item with a narrower bar.
5.Discussion
Analysis of LSP contextual and intermediate outcomes data from six home-based intervention programs in the United States enabled the research team to examine both the extent of MHL improvement and what influenced disadvantaged mothers’ capacity to manage episodic and everyday challenges to family health. Contextual data provided a rare view of the home context in which mothers raising children in poverty use information for health and enabled the authors to probe the complexity of mothers’ everyday lives as a guide to intervention. Results add evidence to findings from previous LSP-MHL studies, highlight the utility of contextual and intermediate outcomes data in health literacy practice and research, and suggest new directions for LSP-MHL research.
5.1.Results confirm that MHL develops and improves
Overall, mothers achieved significant improvements in risk behaviors, preventive practices, and use of health services and community resources, indicating increased knowledge and skills. Figure 1 shows that progress continued throughout the study period with different patterns of change consistent with earlier findings [32].
Further, findings add evidence that improvements can be maintained and built on over an extended period marked by evolving health challenges. The heatmap, Fig. 2, makes evident the developmental nature of health literacy. As mothers’ and children’s needs changed, mothers demonstrated new skills while maintaining progress in other areas. Improvement occurred across the domains of health literacy. These findings support Nutbeam’s theory that the skills to use information and services for health can be developed through usual health promotion efforts [18].
5.2.Web of interaction maps pathways to progress
The Web of Interaction (Fig. 3) underscores the inherent complexity of MHL in everyday life by visualizing the extent and magnitude of correlations among 36 factors that interact to influence mothers’ progress toward optimal health functioning. All the correlations are statistically significant and positive, indicating that gains in one LSP item score correlate with gains in multiple related items. This new finding has significant implications for practice; it means that each item represents a point to start a positive chain reaction.
Data-informed service providers can tailor intervention to address almost any issue that motivates the mother, and reasonably expect to simultaneously or subsequently improve MHL, advance program priorities, and positively influence the health trajectory of the dyad. For example, one mother’s goal to obtain a driver’s license (transportation, a social determinant of health) initially seemed a distraction, but her efforts catalyzed MHL score improvement along with other positive changes. The license enabled her to participate in well-child preventive care, and to get a job, which increased her income and enabled her to provide better nutrition and a safer, more stable and stimulating environment, which in turn increased her self-esteem and capacity to improve risk behaviors and support child development.
5.3.Reading skill is not an important factor in MHL
The Web of Interaction (Fig. 3) shows estimated reading skill is the least influential of 36 factors in MHL. This result confirms a previous LSP-MHL study that found reading skill predicted MHL scores at baseline, but did not predict improvement [30]. Advanced HL skills developed even where functional skills were weak. Focus on developing interactive and critical skills, especially reflection, through a collaborative, mother-directed, problem-focused process consistently improved MHL scores [7,12,16,30].
5.4.Promoting MHL reduces disparities
Unskilled readers made greater progress in MHL than their more skilled counterparts [30], indicating that reading skill is neither necessary nor sufficient to manage health and healthcare. The intervention benefitted skilled and unskilled readers, and also reduced the gap between them. This has not been achieved by information improvement initiatives in child health [8]. Further, previous LSP studies showed reductions in disparities related to age [30] and mental health [16,32].
5.5.MHL promotion empowers women
Previous LSP-MHL studies demonstrated that MHL improvement empowers mothers for health. Two studies [16,32] found that depressed mothers improved their MHL scores in part by obtaining treatment for depression, demonstrating increased understanding of information and services, and increased control over actions and decisions affecting the dyad’s health. Another study found MHL also empowered service providers in three Parents as Teachers programs [7].
The heat map, Fig. 2, further demonstrates empowerment. In the example of prenatal care described under Results, the figure shows a near zero level of prenatal care participation was maintained through the second year of service. The heatmap also shows a strong increase in Family Planning scores in the same period. These two MHL indicators together strongly suggest that, across the six programs, mothers achieved health empowerment as defined by the World Bank [40]: they made a health decision (to plan their next pregnancy); they transformed that choice into desired actions (choose, obtain, use a birth control method) and outcomes (control of their lives and health). These findings further demonstrate health literacy promotion as a pragmatic intervention to empower women and thereby improve infant health and future adult health.
5.6.Data-driven health literacy promotion is feasible and effective
This study demonstrates that data-driven, evidence-based health literacy promotion is feasible and effective. Non-scientist service providers working in uncontrolled home and community environments demonstrated ability to collect quality data, interpret and use it to personalize intervention for specific individuals and circumstances. Paraprofessionals [7,30], social workers [12], and nurse case managers [16] were shown to be effective catalysts to MHL improvement.
5.7.Strong relationships among social determinants of health and MHL
Mobley and colleagues [16] found that rural mothers with low MHL scores had problems with housing and transportation. This finding suggested that the social determinants of health (SDoH) might be significant factors in MHL. In the present study, data visualization made clear the powerful influence of transportation and other SDoH, evidenced in the Web of Interaction by the large footprints of items in the Basic Essentials category. The role of SDoH in health literacy improvement is new vista for future research.
5.8.Integrate MHL promotion into existing interventions
Results confirmed that MHL promotion can be integrated into the goals and usual activities of larger existing preventive interventions. The LSP-MHL studies evaluated implementations of the intervention in nine programs in disparate regions of the U.S. with overlapping goals and various service populations, models and providers. Consistently positive results support MHL promotion as a pragmatic intervention that could be scaled up through existing home-based programs.
5.9.Complexity facilitates intervention
This study challenges earlier LSP-MHL studies which concentrated on health literacy indicators with limited, selective attention to the contextual data. Results demonstrate that the complexity of dynamic, sometimes chaotic home environments does not preclude strategic intervention; nor does it reduce understanding of what impedes or promotes MHL. Rather, the complexity guides and facilitates intervention.
6.New directions in LSP-MHL research and practice
6.1.Analyze outcomes and contextual data together
Future LSP-MHL studies should analyze full contextual data along with MHL indicators to further inform interpretation of findings and increase understanding of what impedes or promotes MHL. More studies are needed to fully understand the relationship of MHL and the SDoH and to evaluate interventions that directly address the SDoH as a strategy to increase capacity for MHL.
6.2.Facilitate routine use of data by service providers
Technology and data visualization should be applied to facilitate routine use of data by non-scientist service providers. Additional studies are needed to determine how data visualization methods can be applied to elucidate progress in particular families, caseloads, and programs, and the degree to which they support evidence-based practice and policymaking by non-scientists.
6.3.Apply implementation science to guide scale-up
The U.S. Affordable Care Act [24] expanded home visitation nationwide, set standards of effectiveness, and required outcomes evaluation to identify promising practices and increase quality of service. This expansion and move to evidence-based practice suggest further evaluation of home visitation networks as existing infrastructure on which to mount a national initiative to improve health literacy in disadvantaged parents and empower women in the United States.
6.4.Update, expand the LSP database
To facilitate such research, the LSP database should be updated and expanded. This can be rapidly accomplished by collecting existing LSP data now held separately by more than 400 programs using the instrument as of early 2017. Early adopters have up to 13 years of data.
An expanded database would overcome a limitation of this and other LSP-MHL studies, and increase their strengths. Additional data on male partners would enable evaluation of paternal health literacy progress. The variety of participating programs and service providers, and the size and diversity of the combined study population, along with repeated measures of intermediate outcomes and contextual factors would provide robust data to better understand and promote MHL and empowerment.
Further, the expanded and updated database would serve as the foundation for a national database to collect data as it is generated and establish norms, comparison groups, and performance reports for contributors. A national LSP database would support ongoing research to rapidly identify and disseminate best practices in MHL promotion, and in home visiting, while training the next generation of researchers for both fields.
7.Post script: Health literacy research and practice for the third era of modern healthcare
This postscript considers two of many implications of the LSP-MHL studies for future health literacy research and practice. First, in the broad view, the author traces the theoretical foundations of the LSP-MHL framework to global health policy, and further to its roots in the convergence of theory and evidence from multiple fields that is bringing heath literacy promotion to the forefront of global health. The potential of future health literacy research grounded in that theoretical foundation is discussed. Secondly, the LSP-MHL intervention studies address a specific identified need for research in health literacy and child health including, in addition to theoretical grounding and evidence, specific strategies and an evaluation framework.
7.1.Theoretical foundations to advance research and practice
Health literacy emerged as a field of research and health policy around 2000. In the same period, theory and empirical evidence from multiple fields converged into a new understanding of health and disease that ushered in the third era of modern healthcare [10]. However, health literacy research has yet to make the shift to the new paradigm. Consequently, two decades of research has produced scant data and little insight to inform intervention. The LSP-MHL studies can serve as a model to help align research with the theoretical foundations of the new era.
7.2.A brief history of healthcare
The first era of modern healthcare (1900s) began with germ theory and understanding of health as the absence of disease. Practice aimed to achieve survival from infectious diseases. The second era (1950–) started with discovery of gene theory and understanding of health as a combination of genetic makeup and adult lifestyle choices. First-era practice was overlaid with chronic disease treatment and emphasis on quality of life, patient activation, informed consent, self-care, and health promotion. The current third era of modern healthcare (2000–) began with discovery of the Developmental Origins of Health and Disease (DOHaD) [38].
Evidence of DOHaD led global health scholars and policy makers to view promoting health literacy as a pragmatic intervention to improve public health, empower women, and reduce disparities worldwide. U.S. policy documents call for health literacy intervention to improve maternal-child health and achieve the full benefits of health care reform [37]. Still, healthcare systems have been slow to respond. Research in U.S. academic medical centers continues to develop the science around second era concepts of health and literacy; an approach that has stymied intervention.
Two theories that grew out of DOHaD underpin the LSP, MHL and global health literacy policy. These theories offer new foundations for research to increase understanding of the broader concept of health literacy and inform intervention to promote it across the life course. Theory-based evaluation combining outcome measures with contextual data can shed light on both the extent of improvement and how the change occurred [29].
7.3.Life course health development – health literacy over the life course
Discovery of DOHaD led to new understanding of health as constantly developing and socially determined. Life course health development theory [9] describes how health develops over a person’s lifetime. The primary challenges and tasks of health protection, promotion, and management evolve along a trajectory from early development in utero and childhood, to increasing function in adolescence, to maintenance of function in adulthood, to decline in old age. Health literacy challenges and skills change along the same trajectory, such that an individual’s health literacy progression is lifelong and evolving; hence, the UN General Assembly’s recommendation to promote health literacy across the life course.
7.4.The social determinants of health – on parents
The Social Determinants of Health (SDoH) are factors that determine whether and how developmental predisposition to adult disease is expressed. Health influences and is influenced first by our parents’ and then our own income, education, nutrition, transportation, and physical and social environments including healthcare access and health literacy [33]. Child development research shows that parents pass skills to their children in the course of everyday interactions [17]. Therefore, the benefits of parents’ improved health literacy can be expected to extend to entire families across their life course; hence the United Nations’ call to focus health literacy promotion efforts on parents. Findings of the latest LSP-MHL study confirm the logic that the SDoH also are determinants of health literacy.
7.5.Health disparities begin before birth – mothers in poverty
Since the social determinants of health shape parents’ health and health literacy, which in turn shape their children’s early development and adult health, disparities are present even before birth and perpetuate. Therefore, health and health literacy follow the social gradient; disease and limited health literacy concentrate among the disadvantaged and disempowered; hence the research priority on parents raising children in poverty. The LSP-MHL studies found that lower functioning mothers made greater gains in MHL than their higher functioning counterparts and so reduced disparities related to literacy, young age, and mental health.
The LSP-MHL studies and other research with parents confirm that mothers remain the primary caregivers of children, and the primary managers of health and healthcare at home [15]. It is likely that fathers have MHL and perhaps other distinctly paternal health literacy skills; but available data on fathers is insufficient to assess those skills or their impacts. Improving MHL, and in the process empowering disadvantaged women, reduces disparities by enabling mothers to reduce health risks, maximize protective factors, and better obtain the benefits of accessible health and social services for themselves and their families.
7.6.Health empowerment – interactive and reflective skills
Health literacy is empowering to the degree that it enables individuals to gain control of decisions and actions that affect their health. The second-era approach to health literacy research and practice views adequate health-related literacy as a prerequisite for health empowerment. Since low health-related literacy is considered to be pervasive and unmodifiable short of reforming education systems, research has generally ignored empowerment. Rather, patients’ low literacy has been posited as an explanation for inequities and disparities, low quality, [2] poor outcomes [6], and high costs [25]. This deficit approach is disempowering to all concerned. It ignores the health literacy of those without current need or access to services. It positions those seeking care as cognitively inadequate or insufficiently motivated to obtain the benefits of that care. Without empowerment, improved understanding of healthcare information fosters dependence on health professionals to decide what to believe or do.
In contrast, in the LSP-MHL approach, service providers engaged mothers in reflection, a process through which mothers honed interactive and critical skills to decide themselves what to believe or do. By definition, they were empowered; they gained control over decisions and actions that affect their health [40].
The LSP-MHL studies show that theory-based evaluation combining intermediate outcomes measures with contextual data can elucidate both the extent of improvement and what facilitated or impeded it. By starting from the understanding that health and disease originate in early development and evolve over the life course in ways determined by social conditions, health literacy research can guide intervention across the life course and so reduce the burdens of disease and disparities worldwide in the third era of modern healthcare.
8.Evidence-based evaluation of health literacy for child health
The LSP-MHL studies address an important specific research need identified by Dewalt and Hink [8]. In a systematic review of health literacy and child health, they found an abundance of information improvement initiatives, but a comparative dearth of evidence-based assessments of interventions to improve parents’ health literacy, especially interventions that reduced disparities between skilled and unskilled readers. In addition to theoretical grounding, the LSP provides evidence, specific strategies, and a comprehensive evaluation framework for community, family, and child health interventions.
8.1.Health promotion strategies improve MHL
Health literacy can be promoted through usual health promotion activities: health education, skills development, and direct information assistance. Health promotion planning typically is concerned with content, timing and teaching strategy. In the LSP-MHL intervention, content and timing are determined by the mother according to her interest and motivation and surrounding family and community conditions. The teaching strategy is reflective questioning.
8.2.Reflective questioning: Teach by asking
Rather than delivering standard content and answering questions, service providers were trained to use LSP data to prioritize needs, build on strengths, and tailor reflective questions to engage mothers in addressing a particular challenge. Reflective questions create opportunities to practice interactive and critical skills in the process of deciding what to believe or do. Reflective conversations led mothers to prioritize challenges, obtain information, plan actions, marshall resources, and progress toward their goals with increasing autonomy and confidence.
8.3.“I talk less; parents think more”
The use of reflective questioning, instead of traditional information-giving or educating, precipitates an essential change in practice. By leading reflective conversations, service providers shifted the focus of their visits from expert-defined content to the reflective process, so that learning became mother-directed, problem-based, collaborative, and therefore empowering. Reflective questioning shifts the intent of health education from information-giving for knowledge gain, to empowerment for making decisions and taking actions that affect health.
Direct information assistance includes reflective conversation to evaluate and personalize information and apply it in context for personal benefit. Mothers were encouraged to discuss information from healthcare providers and other sources. To aid recall, trigger discussion, and encourage further learning, mothers were provided printed health education materials, including materials designed for low-skilled learners [31]. Print materials and other information were offered when requested, rather than according to a schedule, and were discussed as part of reflective conversations. More research is needed to determine the degree of improvement attributable to materials.
9.Evaluation framework for health literacy interventions in child health
What researchers measure and how they measure it matters because it determines what they find out about what works, what is worth doing, and who should do it [29]. The LSP approach to measuring health literacy and evaluating interventions in child health can advance research and practice by changing what researchers measure, how they measure it, and how practitioners use the data.
The dominant clinical approach asks How poorly does this patient read? It measures patients’ and parents’ health-related literacy by a single administration of a brief reading test. From these measures researchers have found out that nearly everyone, including an estimated one third of parents [41], has low health-related literacy. This “silent epidemic” [23] presents a risk to child safety, systems efficiency, and costs. Researchers have concluded that nothing short of reforming education systems can improve parents’ health-related literacy; so improving information is the only available response. As the primary source of knowledge in healthcare organizations, clinicians are expected to manage the risks of parents’ and other patients’ low health-related literacy. Some argue for using the data to identify patients with low health-related literacy; but reading test scores suggest no viable response to those patients. Bennett validated a 3-question screen to identify parents of children to age 6 in pediatric care who would benefit by referral to adult literacy programs [5]. With this exception, health-related literacy testing is conducted only for research purposes since it leaves patients feeling embarrassed and alienated [22], disempowered.
In contrast, the LSP asks What is this mother doing for health? What is helping; and what is in her way? Rather than estimating skill level and inferring what a person at a given level of skill can or will do, the LSP monitors progress to optimal functioning through a continuum of characteristic actions, practices and behaviors indicative of increasing skill and autonomy. From measures of progress, researchers and practitioners see changes in what a mother (or a service population), actually does for health with the information, skills and support she has. With repeated measures, they can see the effects of both improved information and of efforts to increase capacity to use that information.
Since the LSP monitors changes in the home context, researchers and practitioners also gain insight into how the social determinants of health operate to influence a family’s health and health literacy. The contextual data supports recommendations that pediatricians collaborate with home visitation programs [1,3] to monitor and improve child health. It might be more effective to address health and social problems together, rather than through separate systems [12].
By embracing the complexity, researchers find multiple pathways to progress, and multiple points from which practitioners can start a positive chain reaction. The challenge then is not to discover the one thing that works, but rather to discover the combination of factors that work for a particular mother and child in a particular situation. Whatever step a mother is willing and able to take now for her child’s health is worth taking; it shifts her into action, sets the dyad on a positive trajectory, and builds confidence to take the next step.
Further, from measures of progress, researchers find that professional and paraprofessional health and social services providers of diverse backgrounds can be effective catalysts to improve maternal health literacy, and thereby improve child health and future adult health. Action research in health literacy and child health, like the LSP studies, in which practitioners undertake research activities to increase their own effectiveness, hones intervention and might reveal a universal process for identifying the effective combination of factors in a specific circumstance.
While the LSP is a data collection instrument, it also is integral to intervention and its evaluation. The LSP documents progress, regression, and maintenance that otherwise may not be evident, and guides practice in the field. Further, LSP data documents effectiveness for funders and policy makers, guides reflective supervision, and informs staff training and evaluation.
The LSP-MHL studies demonstrate the feasibility and effectiveness of health literacy intervention in child health. Intervention that is grounded in current theory and empirical evidence, community-based, and data-driven can improve maternal health literacy, empower women, and positively influence the health trajectory of families and communities.
10.Third-era health literacy research: Multidisciplinary and multinational
Additional implications of the LSP-MHL intervention studies provide a platform for future multidisciplinary dialogue on the challenges and promises of data-drive practice, evidence-based evaluation, and theory-based research in health literacy promotion, particularly in maternal and child health. Topics for ongoing discussion include incorporating MHL improvement into federal benchmarks of effectiveness in home visitation; how the LSP approach can be adapted for disease-specific home-based interventions and clinical settings; and how implementation science and big data methods can be applied to disseminate MHL promotion in community-based intervention programs. Collaborative multinational research may identify a universal method to adapt the LSP-MHL approach to cultures and conditions in poverty populations across the globe.11
Notes
1 This research was funded by the U.S. National Library of Medicine. The authors declare there is no conflict of interest.
References
[1] | M.A. Abrams, P. Klass and B.P. Dreyer, Health literacy and children: Recommendations for action, Pediatrics 124: (Supplement) ((2009) ), S327–S331. doi:10.1542/peds.2009-1162I. |
[2] | Agency for Healthcare Research and Quality, National Healthcare Disparities Report, U.S. Department of Health and Human Services, Agency for Healthcare Research and Quality, Rockville, MD, (2008) , AHRQ Pub. No. 08-0041. |
[3] | American Academy of Pediatrics, Council on Community Pediatrics, The role of preschool home-visiting programs in improving children’s developmental and health outcomes. Available at www.pediatrics.org/cgi/DOI/10.1542/peds.2008-3607. Retrieved October 4, 2016. |
[4] | D.W. Baker, The meaning and the measure of health literacy, J Gen Intern Med 21: (8) ((2006) ), 878–883. doi:10.1111/j.1525-1497.2006.00540.x. |
[5] | I.M. Bennett, S. Robbins and T. Haecker, Screening for low literacy among adult caregivers of pediatric patients, Fam Med 35: ((2003) ), 585–590. |
[6] | N.D. Berkman, S.L. Sheridan, K.E. Donahue, D.J. Halpern, A. Viera, K. Crotty, A. Holland, M. Brasure, K.N. Lohr, E. Harden, E. Tant, I. Wallace and M. Viswanathan, Health literacy interventions and outcomes: An updated systematic review, Evidence Report/Technology Assessment No. 199, RTI International-University of North Carolina Evidence-based Practice Center under contract No. 290-2007-10056-I. |
[7] | L.N. Carroll, S.A. Smith and N.R. Thomson, Parents as teachers health literacy demonstration project: Integrating an empowerment model of health literacy promotion into home-based parent education, Health Promot Pract 16: (2) ((2014) ), 282–290. doi:10.1177/1524839914538968. |
[8] | D.A. Dewalt and A. Hink, Health literacy and child health outcomes: A systematic review of the literature, Pediatrics 124: (Supplement) ((2009) ), S265–S274. doi:10.1542/peds.2009-1162B. |
[9] | N. Halfon and M. Hochstein, Life course health development: An integrated framework for developing health, policy, and research, Milbank Q 80: (3) ((2002) ), 433–479. doi:10.1111/1468-0009.00019. |
[10] | N. Halfon, K. Larson, M. Lu, E. Tullis and S. Russ, Lifecourse health development: Past, present and future, Matern Child Health J 18: ((2014) ), 344–365. doi:10.1007/s10995-013-1346-2. |
[11] | M. Hanson, P. Gluckman, D. Nutbeam and J. Hearn, Priority actions for the non communicable disease crisis, Lancet 378: ((2011) ), 566–567. Shanghai Declaration is available at http://www.thelancet.com/cms/attachment/2009245863/2032056526/mmc1.pdf. Retrieved October 4 2016. doi:10.1016/S0140-6736(11)61286-5. |
[12] | G.W. Haynes, D. Neuman, C. Hook et al., Comparing child and family outcomes between two home visitation programs, Fam Consum Sci Res J 43: (3) ((2015) ), 209–228. doi:10.1111/fcsr.12098. |
[13] | I. Kickbush and D. Maag, Health literacy, in: International Encyclopedia of Public Health, 3rd edn, K. Heggenhougen and S. Quah, eds, Academic Press, San Diego, (2008) , pp. 204–211. |
[14] | I. Kickbush, J.M. Pelikan, F. Apfel and A.D. Tsouros (eds), Health Literacy: The Solid Facts, World Health Organization, Copenhagen, (2013) . Available at http://www.euro.who.int/__data/assets/pdf_file/0008/190655/e96854.pdf?ua=1. Retrieved October 4, 2016. |
[15] | S. Matoff-Stepp, B. Applebaum, J. Pooler and E. Kavanagh, Women as health care decision-makers: Implications for health care coverage in the United States, J Health Care Poor Underserved 25: (4) ((2014) ), 1507–1513. doi:10.1353/hpu.2014.0154. |
[16] | S. Mobley, S. Thomas, D. Sutherland et al., Maternal health literacy progression among rural perinatal women, Matern Child Health J 18: (8) ((2014) ), 1881. doi:10.1007/s10995-014-1432-0. |
[17] | National Research Council and Institute of Medicine, From Neurons to Neighborhoods: The Science of Early Childhood Development, Committee on Integrating the Science of Early Childhood Development, J.P. Shonkoff and D.A. Phillips, eds, Board on Children, Youth, and Families, Commission on Behavioral and Social Sciences and Education, National Academy Press, Washington, DC, (2000) . |
[18] | D. Nutbeam, Health outcomes and health promotion: Defining success in health promotion, Health Promo J of Austr 6: ((1996) ), 58–60. |
[19] | D. Nutbeam, Health promotion glossary, Health Prom Int 13: (4) ((1998) ), 349–364. doi:10.1093/heapro/13.4.349. |
[20] | D. Nutbeam, The evolving concept of health literacy, Soc Sci Med 67: ((2008) ), 2072–2078. doi:10.1016/j.socscimed.2008.09.050. |
[21] | D. Nutbeam, Defining and measuring health literacy: What can we learn from literacy studies?, Int J Public Health 54: (5) ((2009) ), 303–305. doi:10.1007/s00038-009-0050-x. |
[22] | N. Parikh, R. Parker, J. Nurss, D.W. Baker and M.D. Williams, Shame and health literacy: The unspoken connection, Patient Educ and Couns 27: ((1996) ), 33–39. doi:10.1016/0738-3991(95)00787-3. |
[23] | R.M. Parker and J.G. Schwartzberg (guest eds), What patients do – and don’t – understand: Widespread ignorance has triggered a silent epidemic, Postgrad Med 109: (5) ((2001) ), 13–16. |
[24] | Patient protection and affordable care act, 42 U.S.C. § 18001 et seq., 2010. |
[25] | R.S. Rasu, W.A. Bawa, R. Suminski, K. Snella and B. Warady, Health literacy impact on national healthcare utilization and expenditure, Int J Health Policy Manag 4: (11) ((2015) ), 747–755. doi:10.15171/ijhpm.2015.151. |
[26] | S. Renkert and D. Nutbeam, Opportunities to improve maternal health literacy through ante-natal education: An exploratory study, Health Prom Int 16: ((2001) ), 381–388. doi:10.1093/heapro/16.4.381. |
[27] | RStudio Team, RStudio: Integrated Development for R, R Studio Inc, Boston, (2013) . |
[28] | R.E. Rudd, Mismatch between skills of patients and tools in use: Might literacy affect diagnoses and research?, J Rheumatol 37: (5) ((2010) ), 885–886. doi:10.3899/jrheum.100135. |
[29] | L. Schorr, Common Purpose: Strengthening Families and Neighborhoods to Rebuild America, Anchor Books, New York, NY, (1997) . |
[30] | S. Smith, Promoting health literacy; concept, measurement, intervention, PhD dissertation, Union Institute and University, Cincinnati, OH, 2009. Publication No. AAT 3375168. |
[31] | S.A. Smith, Beginnings Pregnancy Guide and Beginnings Parents Guide, Practice Development Inc, Seattle, (1989) –(2014) . |
[32] | S.A. Smith and E.J. Moore, Health literacy and depression in the context of home visitation, Matern Child Health J 16: (7) ((2012) ), 1500–1508. doi:10.1007/s10995-011-0920-8. |
[33] | Social determinants of health, 2016. Available at https://www.healthypeople.gov/2020/topics-objectives/topic/social-determinants-of-health. Retrieved October 4. |
[34] | K. Sørensen, S. Van den Broucke, J. Fullam, G. Doyle, J. Pelikan, Z. Slonska and H. Brand, Health literacy and public health: A systematic review and integration of definitions and models, BMC Public Health 12: (1) ((2012) ), 80. Available at http://www.biomedcentral.com/1471-2458/12/80. Retrieved February 2 2016. doi:10.1186/1471-2458-12-80. |
[35] | StataCorp, Stata Statistical Software: Release 11, StataCorp LP, College Station, TX, (2009) . |
[36] | S. Sykes, J. Wills, G. Rowlands and K. Popple, Understanding critical health literacy: A concept analysis, BMC Public Health 13: (1) ((2013) ), 150. doi:10.1186/1471-2458-13-150. |
[37] | U.S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion, National Action Plan to Improve Health Literacy, U.S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion, Washington, DC, (2010) . Available at https://health.gov/communication/hlactionplan/pdf/Health_Literacy_Action_Plan.pdf. Retrieved May 18, 2017. |
[38] | P. Wadhwa, C. Buss et al., Developmental origins of health and disease: Brief history of the approach and current focus on epigenetic mechanisms, Sem Repro Med 27: (05) ((2009) ), 358–368. doi:10.1055/s-0029-1237424. |
[39] | L. Wollesen and P.K. Life, Skills Progression: An Outcome and Intervention Planning Instrument for Use with Families at Risk, Brookes, Baltimore, (2006) . |
[40] | World Bank, Empowerment. PovertyNet. Available at http://go.worldbank.org/S9B3DNEZ00. Retrieved June 15 2016. |
[41] | H.S. Yin, M. Johnson, A.L. Mendelsohn, M.A. Abrams, L.M. Sanders and B.P. Dreyer, The health literacy of parents in the United States: A nationally representative study, Pediatrics 124: (Suppl) ((2009) ), S289–S298. doi:10.1542/peds.2009-1162E. |



